Deadly pancreatic cancer originates behind the stomach. It’s hard to detect early, which makes it dangerous. The exact cause isn’t clear, but certain habits and conditions raise your risk. To lower your chances, quit smoking, eat healthy, and see a doctor if you have symptoms like yellow skin or belly pain. This guide explains the causes of cancer of the Pancreas and risk factors to help you stay informed.
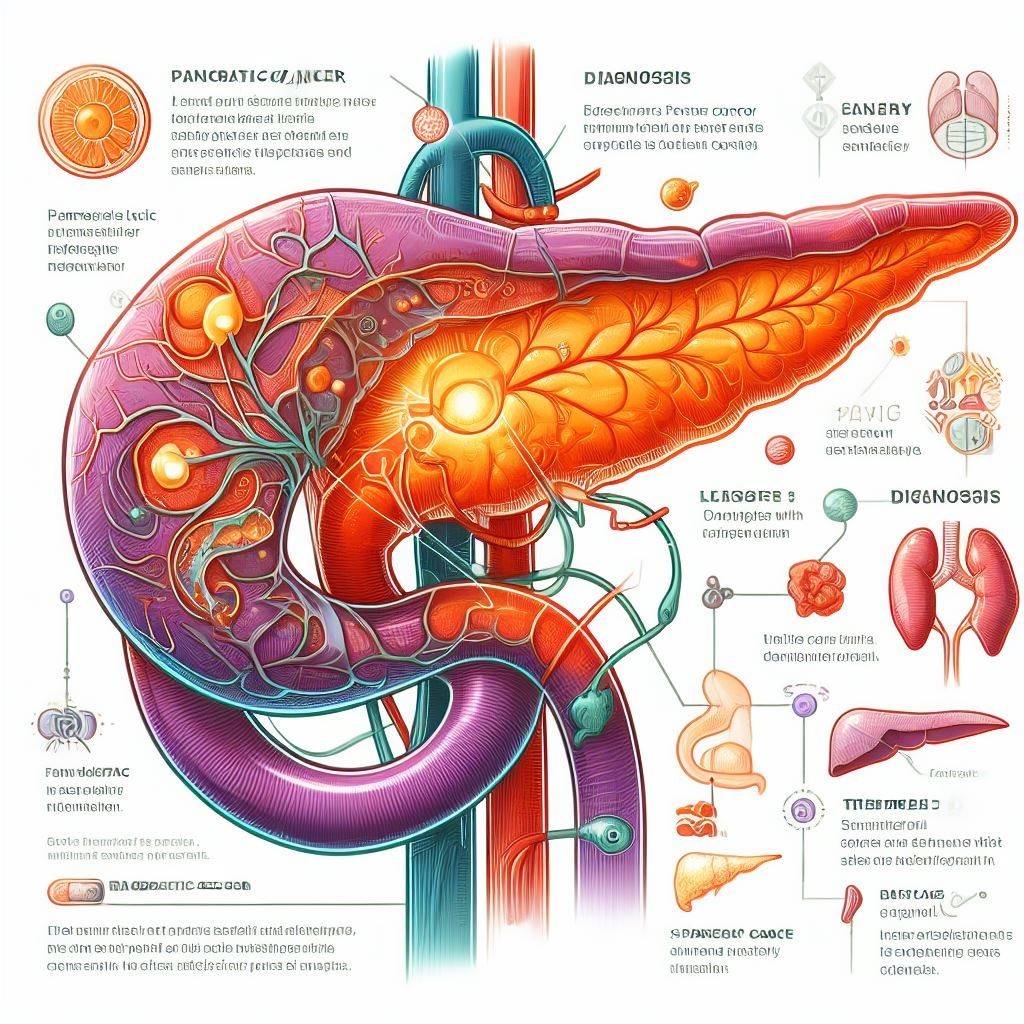
What Is Pancreatic Cancer?
It occurs when cells in the pancreas—the gland vital for digesting food and regulating blood sugar—multiply uncontrollably. I’ve read stories of people who didn’t know they had Cancer of the Pancreas until it was advanced because it’s so muted early on.
Types of Pancreatic Cancer
There are two main types:
- Most pancreatic cancers, like PDAC, arise from digestive juice cells.
- Endocrine tumors arise from hormone-producing cells, like those making insulin; they’re infrequent and less lethal.
Pancreatic carcinoma typically refers to adenocarcinoma of the pancreas, the primary focus here. It’s aggressive and spreads fast.
Why Is Pancreatic Cancer So Dangerous?
It is one of the deadliest cancers. Though it affects only 3% of cases, it results in about 7% of cancer deaths. I find this scary because it shows how tough it is to beat. A mere 5-11% live past five years. What causes this? It is hard to catch early, and it spreads quickly to places like the liver or lungs.
Symptoms to Watch For
Cancer of the Pancreas often has no signs at first. Later, you might notice:
- Yellow skin or eyes (jaundice)
- Pain in the belly or back
- Weight loss without trying
- Feeling exhausted
- Loss of appetite
I’ve seen friends ignore these signs, thinking they’re just stress. Observe these symptoms? Reach out to your doctor without delay. Early intervention saves lives.
What Causes Pancreatic Cancer?
Doctors haven’t pinpointed pancreatic cancer‘s exact trigger yet. It starts when DNA in the pancreas cells changes, making them grow too fast. These changes, or mutations, can happen randomly or from risk factors. I like how researchers are working hard to understand these changes better. [Note: Simplifying science keeps it accessible.]
How Mutations Happen
Cancer of the Pancreas can come from:
- Random DNA errors: When cells divide, mistakes in copying DNA can build up.
- Inherited mutations: Parental gene flaws boost risk.
- Environmental damage: Things like smoking or chemicals harm DNA.
These cancer causes aren’t fully avoidable, but knowing them helps you make smart choices.
Key Risk Factors for Pancreatic Cancer
Risk factors elevate your chances of pancreatic cancer. Certain habits, like smoking, are changeable. Others, like age, you can’t. I’ve seen families worried about Pancreatic Neoplasm risk factors after a loved one’s diagnosis. Let’s break them down.
Modifiable Risk Factors
You can control these cancer of the Pancreas risk factors:
Smoking
Smoking doubles your risk of pancreatic cancer. Tobacco use drives 25% of pancreatic cancer cases—even vaping harms this vital organ. I’ve watched ex-smokers reclaim their health.
Quick fix: Quit now to protect your pancreas.
Obesity
Being overweight raises your risk by 20%. Belly fat is especially risky.
I like eating more vegetables, and walking daily can help with weight management.
Eat right and exercise to manage your weight..
Alcohol
Heavy drinking can cause chronic pancreatitis, which raises Pancreatic Cancer.
I’ve noticed that cutting back on alcohol helps people feel better overall.
Pro tip: Limit alcohol to two drinks max daily
Diet
Overloading on processed meats (think bacon, sausages) boosts disease risks
I love swapping burgers for grilled fish or beans for healthy eating.
Tip: Eat more fruit, veggies, and whole grains.
Non-Modifiable Risk Factors
These pancreatic cancer risk factors are fixed.
Age
Most cases happen after age 65. Most diagnoses occur at age 70.
I’ve seen older relatives get regular checkups to stay proactive.
Gender
Men exhibit a slightly higher risk of pancreatic cancer than women.
Some say this is because men smoke more, but it’s not the whole story.
Race
Ashkenazi Jews and Black Americans face elevated risks.
The reasons aren’t clear, but diabetes and obesity may play a role.
Family History
If a parent or sibling had Pancreatic Cancer, your risk is higher.
I’ve seen families get genetic testing to understand their risk better.
Inherited Gene Mutations
Genes like BRCA2 or PALB2 increase risk.
Lynch and Peutz-Jeghers syndromes also heighten risk.
Family cancer history? Consult a genetic counsellor.
Medical Conditions Linked to Pancreatic Cancer
Some health problems make a Malignant Pancreatic Tumor more likely. I find it surprising how connected our body systems are.
Chronic Pancreatitis
Chronic pancreatitis is a long-term inflammation. It’s often caused by heavy alcohol use or smoking. It raises Pancreatic Carcinoma significantly.
Tip: Avoid heavy drinking and smoking to protect your pancreas.
Diabetes
Type 2 diabetes doubles Pancreatic Carcinoma. Sometimes, it causes late-onset diabetes. I’ve seen doctors check for cancer of the Pancreas when older adults suddenly get diabetes.
Tip: Manage blood sugar with diet and exercise.
Other Conditions
Genetic rarity: Hereditary pancreatitis sparks chronic pancreatic inflammation.
Cystic fibrosis causes pancreatic problems and a higher cancer of the Pancreas.
Tip: If you have these, ask your doctor about screening.
Emerging Risk Factors
New research is finding more cancer of the Pancreas. I’m eager about these discoveries because they could lead to better prevention.
Gut Bacteria
Gut microbiota may affect cancer of the Pancreas. Unhealthy bacteria, like those from gum disease or H. pylori infections, might play a role. I’ve started brushing twice a day to keep my mouth healthy!
Tip: Good oral hygiene may help lower the risk.
Blood Type
People with non-O blood types (A, B, or AB) may have a slightly higher cancer of the Pancreas. I find this fascinating because it’s such a minor detail!
Tip: You can’t change your blood type, but knowing this can prompt checkups.
Lipid Levels
High cholesterol or triglycerides may increase Pancreatic Malignancy. I like checking my cholesterol yearly to stay on top of it.
Tip: Eat heart-healthy foods like oats and nuts.
How to Lower Your Pancreatic Cancer Risk.
You can’t prevent cancer of the Pancreas completely, but you can reduce your risk factors. I’ve seen small changes make a big difference in people’s health.
Lifestyle Changes
Quit Smoking
Use support, like apps or counselling. I’ve seen friends quit with help from quit lines.
Stay Active
Aim for 30 minutes of walking most days. I love how walking clears my mind.
Eat Healthy
Choose fruits, veggies, and lean proteins over processed foods.
Limit Alcohol
Stick to moderate drinking to avoid pancreatitis.
Screening for High-Risk People
If you have a family history or genetic mutations, screening can catch cancer of the Pancreas early. Tests like MRI or endoscopic ultrasound help. I’ve seen families feel relieved after getting screened.
Tip: Ask your doctor about genetic counselling if Pancreatic Cancer runs in your family.
FAQS About Pancreatic Cancer
What is the biggest cause of Pancreatic Cancer?
Smoking is the top modifiable risk factor, causing about 25% of cases. Genetic mutations also play a role.
Can you prevent Pancreatic Cancer?
Not fully, but quitting smoking, staying at a healthy weight, and limiting alcohol lowers your Cancer of the Pancreas risk factors.
Who is most at risk for Pancreatic Cancer?
People over 65, smokers, and those with a family history or Type 2 diabetes have the highest risk.
Does diet affect Pancreatic Cancer risk?
Yes, eating red or processed meat may raise the risk, while fruits and veggies may lower it.
Final Thoughts
Pancreatic Cancer is a tough disease, but understanding its causes and risk factors can help you take control. I’ve seen how quitting smoking or eating better can make people feel empowered. Make minor changes like walking daily or seeing a doctor if you notice symptoms. If Cancer of the Pancreas runs in your family, talk about screening. You’ve got this—stay informed and stay healthy.