Navigate the challenges of Diabetes and Stomach Issues with our practical guide. Learn effective strategies for relief and proactive management. Explore now!
Introduction to Diabetes and Stomach Issues

If you have diabetes, you may also struggle with diabetes and stomach issues like digestive problems, abdominal discomfort, or gastrointestinal complications. High and unstable blood sugar levels can wreak havoc on your stomach and gut health over time.
Managing these annoying or painful diabetes stomach issues is critical for maintaining nutrition and optimal quality of life. The good news is that relief is possible through lifestyle changes, medications, specialist care, and other evidence-based treatment strategies.
This practical guide breaks down the common links between diabetes and digestive health. You’ll learn how to recognize symptoms, discover potential causes, and take control with comprehensive management plans for resolving stomach problems.
Read more about: How to Keep Diabetes Under Control: Mastering Your Blood Sugar
How Diabetes Affects Your Digestive System
Uncontrolled high blood sugar from diabetes progressively damages nerves and small blood vessels throughout the body. This includes supplying oxygen and neurological signals to your gastrointestinal (GI) tract.
Constricted blood flow and impaired nerve communication impede digestion from food breakdown to nutrient absorption and waste elimination.
Additionally, diabetes and associated stomach issues may stem from:
- Medication side effects
- Dehydration from frequent urination
- Yeast or bacterial infections
- Increased gut inflammation
- Emotional stress and anxiety
This multifaceted attack on your digestive system explains why so many people with diabetes deal with uncomfortable stomach and gut dysfunction.
Common Types of Diabetes and Stomach Issues
There are several primary types of stomach problems linked to diabetes, ranging from bothersome to severe:
Diabetic Gastroparesis
This nerve damage condition delays the emptying of food contents from your stomach to the small intestine. Symptoms include:
- Nausea
- Vomiting
- Feeling full shortly after starting a meal
- Heartburn
- Bloating
- Stomach pain
Diabetes-Related Diarrhea
Frequent loose, watery stools cause urgency, leakage, and skin irritation. Contributing factors involve:
- Bacterial infections
- Nerve injury
- Medication effects
- Sugar alcohol sweeteners
Diabetes and Constipation Issues
Hard, dry stools become difficult to pass, caused by:
- Dehydration
- Medications that slow motility
- Autonomic neuropathy
- Low fiber intake
Diabetes and GERD
Gastroesophageal reflux disease (GERD) allows stomach acid to damage the esophagus, provoking:
- Heartburn
- Regurgitation
- Chest pain
- Chronic cough
- Trouble swallowing
Pay attention to any new or worsening GI symptoms that develop around your diabetes diagnosis or medication changes. Track your health history closely so providers can determine appropriate solutions.
Signs of Digestive Trouble to Watch For
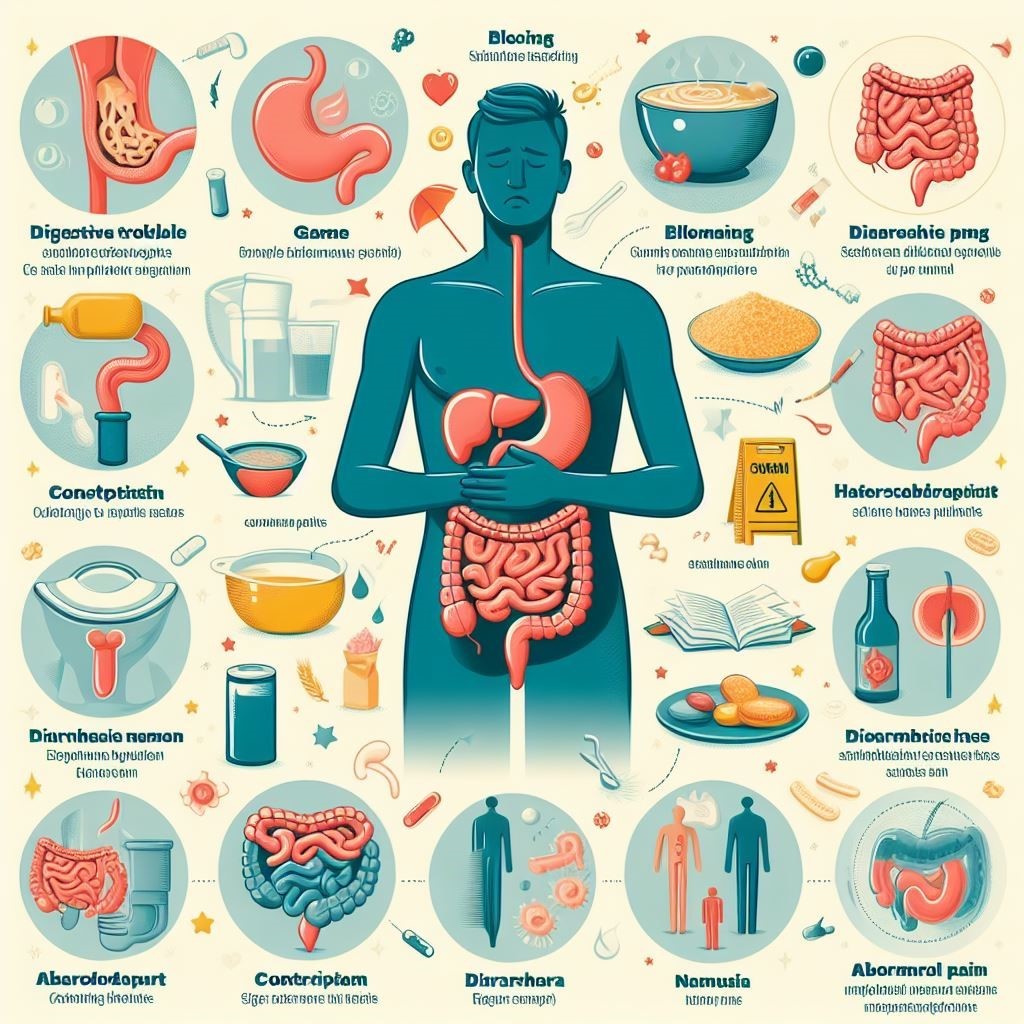
Look out for these common indicators of diabetes and stomach issues:
- Bloating
- Loss of appetite
- Blood sugar level fluctuations
- Abdominal pain or cramping
- Nausea and vomiting
- Diarrhea and/or constipation
- Heartburn
- Unexplained weight loss
Monitor symptoms in a daily journal, diet, and other health details. Share this log with your doctor to help uncover whether digestion difficulties are linked to uncontrolled glucose, medicines, emotional stress, or eating triggers.
Pinpointing causes is key to finding the right treatment approach.
Why Testing Matters for Diabetes and Stomach Issues
If troubling digestive symptoms affect your daily function and diabetes control, your doctor can order tests to inspect for underlying problems.
Diagnostic testing options include:
- Blood tests to check for anemia, markers of infection or inflammation.
- Hydrogen breath testing for carbohydrate intolerance.
- Endoscopy to visually inspect the stomach and esophagus tissue.
- Gastric emptying scan to measure gastroparesis severity.
- Stool analysis to test for blood, improper digestion, or infection.
These tests help uncover issues like bacterial overgrowth, gastroparesis, acid reflux damage, and nutrient malabsorption, interfering with your digestion and diabetes management.
Can Diabetes Medications Contribute to Stomach Issues?
Along with diabetes itself disrupting digestion, some glucose-lowering medications also provoke adverse stomach issues as side effects.
For instance, metformin, GLP-1 medications, SGLT2 inhibitors, and synthetic amylin drugs frequently cause:
- Diarrhea
- Nausea
- Vomiting
- Loss of appetite
- Stomach pain
If symptoms emerge after recently starting a new diabetes med, talk to your doctor. Adjusting dosage or switching prescriptions often relieves medication-related digestive issues.
Lifestyle Changes to Improve diabetes and stomach issues.

While medicines treat underlying causes, making certain daily lifestyle changes empowers you to take control of rebalancing digestive health.
Control Blood Sugar
Getting A1c close to or below 7% prevents extensive nerve damage and vascular disease from interfering with digestion.
Follow Proper Nutrition
A balanced diabetes diet with small, gentle-on-gut meals supports function. A dietitian can tailor eating guidance to your needs.
Stay Hydrated
Dehydration from frequent peeing aggravates GI issues. Sip fluids throughout the day.
Minimize Stress
Anxiety taxes digestion tremendously. Try relaxing practices like yoga, meditation, or speaking with a counsellor.
Exercise in Moderation
Light walking aids digestion, but intense workouts can provoke stomach distress.
Limit Alcohol and Quit Smoking
Both exacerbate gastrointestinal symptoms and related diabetes complications.
Medical Management Options for Diabetes Stomach Problems
If lifestyle measures alone don’t resolve unpleasant digestive symptoms, medications and other conventional or complementary therapies provide relief.
Medications
Popular options treat heartburn, nausea, bowel issues, gastroparesis, and pain.
Gut-Brain Therapies
Relaxation techniques, cognitive behavioral therapy, and antidepressants calm GI distress.
Alternative Treatments
Some patients find symptom relief from probiotics, supplements, essential oils, or acupuncture.
Gastric Electrical Stimulation
Surgically implanted neurostimulator help difficult diabetic gastroparesis cases.
Pay attention to medication side effects and tailor treatments based on effectiveness for your symptoms.
Treatment for Diabetes and Stomach Issues

1: Controlling blood glucose levels prevents further nerve and vessel injury, affecting digestion.
2: Medication changes treat diarrhea or nausea side effects, worsening stomach issues.
3: Dietary changes help ease symptoms – smaller meals, gentle foods.
4: Reducing anxiety and stress through counselling and relaxation practices supports gut health.
5: Medicines like antacids, antidiarrheals, laxatives, and probiotics manage symptoms.
6: Doctors can refer patients with persistent problems to GI specialists for advanced testing and treatments.
Getting Specialist Help for Diabetes and Stomach Issues
If you continue struggling with diarrhea, constipation, nausea, gastroparesis, or other gastrointestinal problems despite self-care efforts and standard drugs, getting a referral to a gastroenterologist (digestive specialist) significantly improves the odds of resolving frustrating stomach issues.
These experts can run in-depth tests to uncover less obvious causes, detect tissue damage early, and walk you through advanced treatments like gastric electrical stimulation for medically refractory symptoms.
Having a knowledgeable gastroenterology specialist in your corner prevents diabetes-related digestive health issues from deteriorating your nutrition and well-being. Getting specialty insight makes a tremendous difference.
Outlook for Overcoming Diabetes and Stomach Problems
Got it. Here is that paragraph simplified and with the keyword inserted twice more:
Battling the dual challenges of diabetes and stomach issues can feel overwhelming. However, getting testing, custom treatment plans and specialist help gives you a chance of resolving or managing common diabetes stomach problems.
Work with your healthcare team to find the right lifestyle changes and therapies to reduce your worst symptoms. Options like diet changes, stress relief, medicines, and nerve stimulation can improve digestive comfort and quality of life.
While diabetes and gastrointestinal issues are often connected, you can control aggravating symptoms and prevent serious complications through consistent self-care and advanced treatments.
Focus on what you can manage with healthy daily habits and working closely with your medical providers. Although occasional flares happen, you can still live fulfilling lives when your diabetes and stomach issues are stabilized.
FAQs about diabetes and stomach issues
Here are the common questions about diabetes and stomach issues, and the best answers.
How does diabetes affect the stomach?
High blood sugar can damage nerves and blood vessels over time. This includes those supplying the stomach and intestines. So diabetes disrupts digestion at multiple points – slowing food breakdown, nutrient absorption, waste removal, etc. These issues cause symptoms like nausea, vomiting, diarrhea, constipation, bloating, and pain.
What are the symptoms of bowel problems with diabetes?
Common signs of diabetic bowel or digestive issues include diarrhea, constipation, gas, bloating, stools with blood or mucus, urgent need to have a bowel movement, feeling you can’t empty your bowels, and cramping or pain.
Can stomach problems cause high blood sugar?
Yes, gastrointestinal problems themselves, as well as treatments, can raise blood sugar levels. For example, infection and inflammation alter insulin uptake. Diarrhea leads to loss of blood glucose in stools. Medications like steroids may trigger hyperglycemia as a side effect.
What are the gastrointestinal complications of diabetes mellitus?
Frequent complications involve gastroparesis (delayed stomach emptying), diarrhea, constipation, dyspepsia, gastroesophageal reflux disease (GERD), abdominal pain, gallstones, impaired nutrient absorption leading to deficiencies, cancers like pancreatic cancer, nonalcoholic fatty liver disease, and problems linked to celiac disease or irritable bowel syndrome.

Adel Galal is a health and wellness writer with over 30 years of experience studying and writing about health, fitness, nutrition, and healthy living. He is the founder of NextFitLife.com, where he shares practical, evidence-based guidance to support long-term health at any age. Adel’s mission is simple:
to help people make smarter health choices that fit real life, at any age.