Diabetes type 2: causes, treatment, and prevention
Explore the causes, treatment, and prevention of diabetes type 2. Empower yourself with the knowledge to manage your health effectively.
Introduction
Explore the causes, treatment, and prevention of type 2 diabetes in this comprehensive guide. Learn about managing type 2 diabetes effectively. It is a disease that lasts for a long time and is caused by too much glucose in the blood. High blood sugar (glucose) is the hallmark of type 2 diabetes, also known as non-insulin-dependent diabetes. Problems arise when the body can’t use and retain glucose correctly. Insulin-resistant diabetes is a devastating disease affecting tens of millions of individuals worldwide. It is possible to enhance one’s health and quality of life by learning about the condition, its risk factors, and its symptoms and then taking action to avoid or treat it. You can control and prevent Insulin-resistant diabetes through regular doctor visits, maintaining a healthy diet, exercising, and achieving a healthy weight.
The root cause of Diabetes type 2
Most people diagnosed with Insulin-resistant diabetes do so for one of two primary causes that are intricately connected.
1- Insulin-sensitive cells in muscle, fat, and the liver change into insulin-resistant cells.
Because these cells interact with insulin, they can’t absorb enough sugar.
2- The pancreas can’t make enough insulin to keep sugar in the blood at a healthy level.
We don’t know why this happens, but being overweight and not getting enough exercise are two significant factors.
However, it is recognized that a mix of hereditary and lifestyle variables is associated with developing Insulin-resistant diabetes.
The specific cause of type 2 diabetes is not entirely understood.
Symptoms that indicate you may have Diabetes type 2
It is a long-term disease when the body doesn’t make enough insulin or the cells don’t respond well to insulin. Diabetes type 2 is a chronic disorder that develops when the body doesn’t create enough insulin, or the cells don’t respond adequately. Both of these factors might contribute to the development of type 2 diabetes. Both of these factors might contribute to the development of type 2 diabetes. This causes the amount of sugar in the blood to go up. Type 2 diabetes symptoms tend to occur slowly over time and can be hard to notice. So many people with the disease may not know they have it. These are some of the most common signs of type 2 diabetes:
More thirst and the need to urinate
As the body tries to eliminate too much sugar through the urine, people with diabetes may feel thirstier and have to go to the bathroom more often, especially at night.
Fatigue
A high blood sugar level can cause symptoms such as a lack of energy and weariness.
This is because cells in the body can’t use sugar to make energy as well as they could.
A fuzzy vision
High blood sugar can make the eye’s lens swell, making it hard to see.
Wounds don’t heal quickly.
Diabetes can make it hard for cuts, sores, and other wounds to heal because it can affect the blood flow and immune system.
Frequent infections
High blood sugar can weaken the immune system, making the body more likely to get infections, especially on the skin, urinary tract, and gums. Symptoms include tingling or numbness in the extremities: If your blood sugar levels are high for a long time, you could damage your nerves, which can cause tingling or numbness in the extremities, like the hands and feet.
Unplanned weight loss
Because the body can’t use sugar for energy, some people with type 2 diabetes may lose weight without effort. It’s important to remember that not everyone with type 2 diabetes will have all these symptoms, and some may have none. So, if you are worried about diabetes or think you might have it, you should talk to a medical professional.
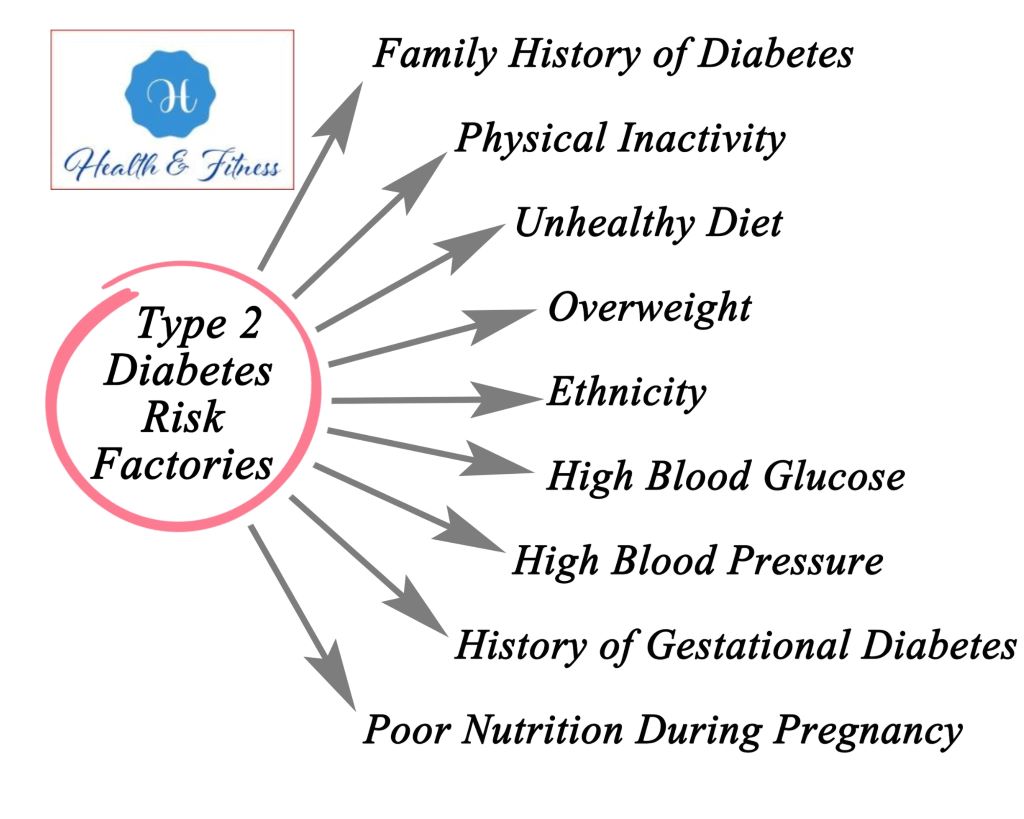
Diabetes type 2 risk factors
Mishandling Type 2 diabetes, a long-term condition, can lead to severe problems, impacting multiple organ systems. These problems include:
Cardiovascular disease
Heart diseases People with Type 2 diabetes are more likely to have health problems like heart attacks and strokes.
Diabetes can hurt the nerves and blood vessels that keep the heart and blood vessels working properly.
Nephropathy (a disease of the kidneys)
High blood sugar can hurt the tiny blood vessels in the kidneys, leading to kidney disease or death.
Neuropathy (nerve damage)
Diabetes can damage nerves, making it hard to feel things in the hands and feet or numb them.
It can also cause pain and make muscles weak.
Retinopathy, or damage to the eye
High blood sugar can damage the blood vessels in the eyes, making it hard to see or even making you go blind.
Foot damage
Damage to the nerves and blood vessels in the feet can be caused by diabetes. This makes it harder for cuts and sores to heal. If this isn’t taken care of, it can increase the chance of amputation.
Skin problems
People with diabetes are more likely to have skin problems like itching and infections.
Dental problems
People with diabetes are more likely to have dental problems like gum disease or lose teeth.
Depression
People with diabetes are more likely to become depressed because of the emotional and physical stress of caring for the disease. It’s important to remember that these complications can often be avoided or put off with good diabetes management, which includes eating well, staying active, and taking medications as prescribed. Regular checkups with a doctor or nurse can also help find and monitor problems.
Diabetes type 2 treatment

Managing blood sugar levels often involves a combination of lifestyle modifications and medication to treat Type 2 diabetes. The particular treatment strategy will vary according to the individual’s diabetes severity. Here are the primary treatment steps for type 2 diabetes:
Lifestyle changes
Changing one’s lifestyle to enhance blood sugar control is one of the most crucial parts of treating Type 2 diabetes.
This could mean losing weight through a healthy diet and regular exercise, giving up smoking, or drinking less.
Medications
Depending on the individual’s needs, a doctor may give you medicine to help you control your blood sugar.
Among the most commonly used drugs to treat Type 2 diabetes is: Metformin is a drug that lowers blood sugar by making the liver make less sugar and making the body more sensitive to insulin. Sulfonylureas: These drugs boost the amount of insulin the pancreas produces. DPP-4 inhibitors: These drugs cause the pancreas to make more insulin and make it harder for carbs to be absorbed from the digestive tract. GLP-1 receptor agonists: These drugs lower the sugar in the blood by making the pancreas produce more insulin and making it harder for the intestine to absorb carbohydrates.
Monitoring
Regular blood sugar monitoring is crucial for someone with type 2 diabetes. You can achieve this by self-testing at home or visiting a healthcare practitioner’s office.
Regular checkups
Monitoring diabetes and its potential consequences requires routine visits to a healthcare expert. They will also assist in modifying the treatment plan as necessary.
Education:
There needs to be education for people with type 2 diabetes on the condition, how to care for those with it, and the complications that can arise. And the prevention of complications. Remember that treatment programs must be individually tailored and that treatment aims to achieve optimal blood sugar control while limiting the risk of complications. To effectively manage diabetes and make any required revisions to treatment programs, it is essential to collaborate closely with a healthcare expert.
When should I schedule a medical appointment?
When you are sick, you need to monitor your diabetes levels closely. The typical cold becomes deadly when insulin and blood sugar are thrown off. Create a “sick day plan” with your doctor that details your routine, how often you should take your medications, and how often you should check your blood sugar levels. If you experience: Contact your doctor immediately if you experience disorientation or memory loss. An internal temperature of 100 degrees or more. Consistently high blood sugar levels for more than a day. Nausea and vomiting that lasts more than four hours, issues with equilibrium or coordination excruciating discomfort all over your body. Lack of mobility in your arms and legs
Type 2 diabetes prevention

You can avoid Insulin-resistant diabetes by lowering risk factors and making healthy lifestyle choices. The onset of Insulin-resistant diabetes can be averted by following these guidelines. Retaining a healthy body mass index Overweight people have a much higher risk of developing Insulin-resistant diabetes. An individual’s chance of acquiring the disease is inversely proportional to their body mass; therefore, losing weight through good nutrition and regular physical activity can help.
We are maintaining a healthy diet.
Eating many whole foods like fruits, vegetables, whole grains, and lean meats makes you less likely to get Insulin-resistant diabetes.
Activity schedules that include
By reducing blood sugar levels and increasing insulin sensitivity, type 2 diabetes is less likely to happen if you work out regularly.
It would be best if you stopped smoking.
Smoking increases the risk of developing Type 2 diabetes. Fortunately, you can reduce this risk by quitting smoking.
No alcohol intake
Moderate alcohol use has lowered the risk of acquiring Insulin-resistant diabetes.
Reducing anxiety:
The chance of getting Insulin-resistant diabetes is raised when stress causes blood sugar levels to rise. Healthy ways to deal with stress, like regular physical activity, yoga, or meditation, can lower the chance of getting the disease.
Routine checkups
By visiting a doctor often, you can catch any potential problems with your health, including Type 2 diabetes, early on.
Keep an eye on your blood sugar.
Regular blood sugar monitoring can help detect diabetes at its earliest stages so treatment can begin immediately.
Modifying your diet and increasing your exercise frequency has demonstrated the ability to decrease the risk of Type 2 diabetes and enhance your overall health. If you have questions or are concerned that you may be at risk for getting diabetes,
you must consult a healthcare provider.
Conclusion
Type 2 diabetics don’t produce enough insulin and can’t use sugar efficiently. Blood glucose rises. High blood sugar is dangerous. Type 2 diabetes is manageable. Exercise and a balanced diet can help control blood sugar.
Insulin may also be needed. Type 2 diabetics must regularly check their blood sugar and communicate with their doctors.
Reference
Diabetes UK” – Official website of a leading diabetes charity in the UK. Website: www.diabetes.org.uk
“NHS: Type 2 diabetes” – Information about Type 2 diabetes from the UK’s National Health Service. Website: www.nhs.uk/conditions/type-2-diabetes