Discover the intricate link between pancreatitis and diabetes. Learn how this connection affects your health and what steps you can take.
Key Takeaways about Pancreatitis and Diabetes
| Term | Definition |
| Pancreatitis | Inflammation of the pancreas that can be acute or chronic |
| Diabetes | Condition caused by high blood sugar levels because of lack of insulin or insulin resistance |
| Connection | Pancreatitis can cause diabetes by damaging insulin-producing cells. Diabetes can also increase the risk of pancreatitis. |
| Management Tips | Control blood sugar, avoid alcohol, and get pancreatitis treatment if needed |
Pancreatitis and diabetes have an intertwined relationship. Understanding the connection between these conditions can help you manage your health if you have one or both. This comprehensive guide covers everything you need to know about pancreatitis and diabetes.
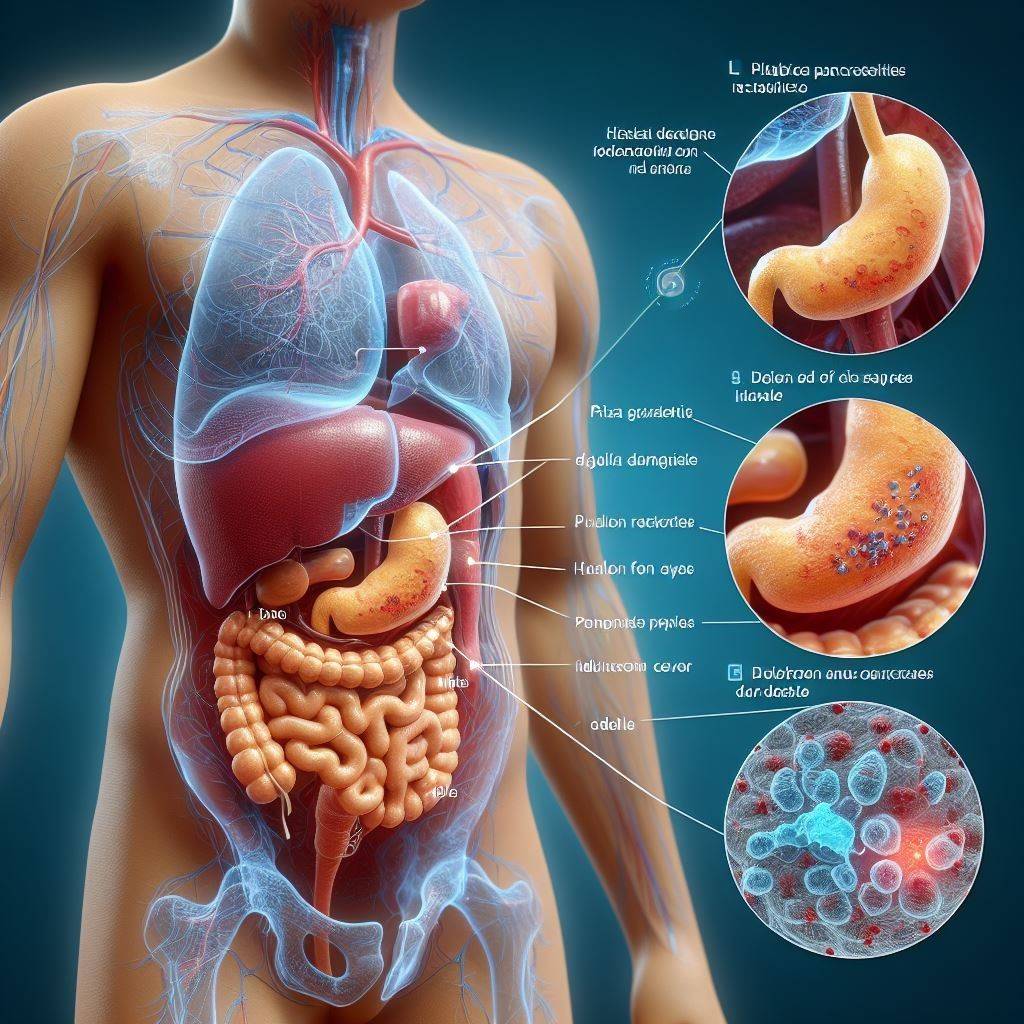
What is pancreatitis?
The pancreas is an organ behind the stomach that produces enzymes that help digest food and hormones like insulin that regulate blood sugar.
Pancreatitis refers to inflammation of the pancreas that impairs its ability to function properly. There are two main types of pancreatitis:
- Acute pancreatitis – Sudden inflammation that develops quickly and lasts for days or weeks.
- Chronic pancreatitis – Ongoing inflammation that causes permanent pancreatic damage over time.
In acute pancreatitis, the pancreas becomes inflamed. This leads to abdominal pain, nausea, vomiting, and fever. Mild cases often resolve on their own, while severe cases can cause serious complications.
With chronic pancreatitis, repeated bouts of acute inflammation cause scarring and irreversible damage to the pancreas. This results in worsening digestion problems and diabetes over time as insulin-producing cells are destroyed.
Overview of Diabetes
Diabetes is a condition characterized by high levels of sugar (glucose) circulating in the bloodstream. This happens for one of two reasons:
- Type 1 diabetes – The immune system mistakenly attacks and destroys insulin-producing cells in the pancreas. Without enough insulin, the body cannot properly move sugar from the blood into cells.
- Type 2 diabetes – The body becomes resistant to the effects of insulin, and the pancreas can’t produce enough insulin to overcome this resistance.
In both types of diabetes, the lack of functional insulin results in blood sugar building up to dangerous levels instead of being used for energy. This can lead to an array of complications if not managed well.
The Link Between Pancreatitis and Diabetes
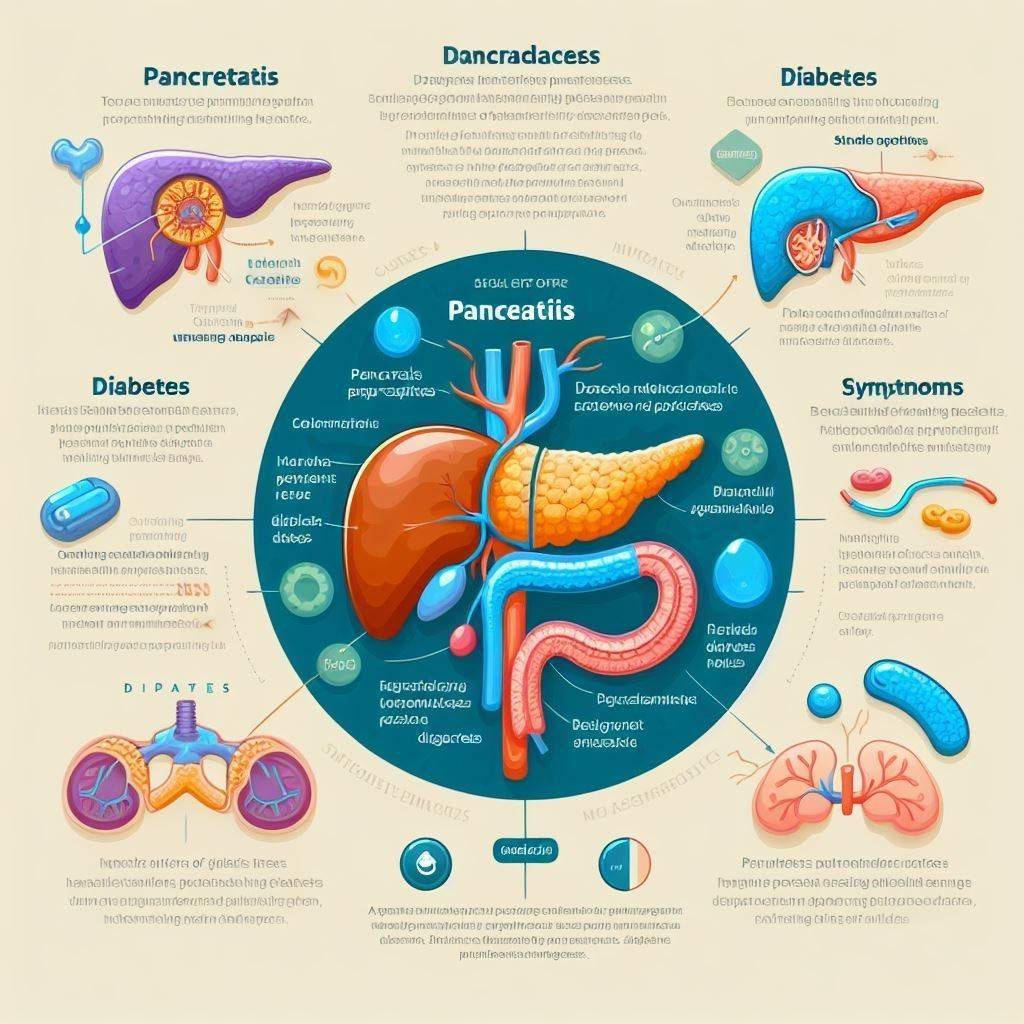
So how are pancreatitis and diabetes connected? There are a few key ways that these conditions can influence each other:
-
Pancreatitis Can Lead to Diabetes
One of the main jobs of the pancreas is to produce insulin. When the pancreas becomes damaged from inflammation, it can disrupt its ability to release insulin properly. Specifically:
- Acute pancreatitis causes swelling that temporarily blocks insulin secretion.
- Chronic pancreatitis permanently destroys insulin-producing cells.
Reduced insulin production means diabetes is more likely to develop. One study found people with chronic pancreatitis had a nearly 4x higher risk of developing diabetes.
-
Diabetes Can Increase the Risk of Pancreatitis
On the flip side, diabetes also seems to predispose people to pancreatitis through a couple of mechanisms:
- Insulin resistance – Impaired insulin signalling can promote inflammation throughout the body, including in the pancreas.
- High blood sugar – Excess sugar can damage blood vessels and organs like the pancreas over time.
One analysis found people with diabetes have double the risk of acute pancreatitis compared to the general population. The risk is even higher for those with type 2 diabetes.
-
Pancreatitis Can Worsen Diabetes
For those who already have diabetes, an episode of acute pancreatitis can complicate managing blood sugar levels. Inflammation impairs the pancreas and reduces insulin production.
One study found over half of diabetics hospitalized for pancreatitis were left with worse glycemic control. Their blood sugar spikes were higher and lasted longer because of inadequate insulin secretion.
So, in summary, the relationship between pancreatitis and diabetes goes both ways. Each condition can influence the onset and severity of the other.
Tips for Pancreatitis and Diabetes
If you have either pancreatitis or diabetes, being aware of their interconnection is key for proper management. Here are some tips:
- Control your blood sugar – Keeping glucose levels stable helps prevent flares of pancreatitis if you have diabetes. Avoid spikes by monitoring levels, taking medication as prescribed, and making diet changes.
- Limit alcohol – Drinking alcohol, especially heavily, is a major cause of pancreatitis. Avoid alcohol or drink only occasionally and in moderation if you have diabetes or pancreatitis.
- Get treatment – See a doctor promptly if you have symptoms of pancreatitis, like abdominal pain. Treating it quickly can help limit any impacts on diabetes management.
- Take prescribed enzymes – If you have chronic pancreatitis, replacing digestive enzymes can help your body absorb nutrients better to stabilize blood sugar.
- See an endocrinologist – Having both a gastroenterologist and an endocrinologist to manage pancreatitis and diabetes together is advisable.
The bottom line is being proactive with your health by following medical advice, testing blood sugar routinely, avoiding triggers, and communicating with your healthcare team. Careful management of both conditions in tandem is crucial.
More on Pancreatitis Symptoms and Diagnosis
Recognizing the signs of pancreatitis is an important part of getting treatment promptly if diabetes and pancreatic problems are a concern for you:
- Abdominal pain – Pain often starts suddenly in the upper abdomen and radiates to the back. It may be mild or severe.
- Nausea and vomiting – These are common as the inflamed pancreas presses on the stomach.
- Fever – A mild fever commonly accompanies pancreatitis.
- Bloating – Abdominal bloating can happen as digestive enzymes leak into the abdomen.
- Fatty stool – The stool may appear greasy and float because of inadequate digestion and absorption of fats.
- Jaundice – Some people develop yellowed skin and eyes as bilirubin builds up.
- Blood sugar changes – Uncontrolled blood sugar is common with pancreatitis.
Pancreatitis is typically diagnosed using:
- Medical history – The doctor will ask about risk factors and symptoms.
- Physical exam – Tenderness when pressing on the abdomen may indicate pancreatitis.
- Blood tests – Markers like amylase and lipase may be elevated.
- Imaging – An MRI, CT scan, or ultrasound can confirm pancreas inflammation.
- Additional tests – Glucose monitoring and endoscopy of the pancreas may be performed.
Treating Pancreatitis
Treatment for pancreatitis involves:
- IV fluids – Fluids and electrolytes are given through the vein to prevent dehydration.
- Pain management – Medications are used to relieve abdominal pain.
- Bowel rest – No food or water from your mouth for a few days to give the pancreas a break.
- Nutritional support – Tube feeding or total parenteral nutrition provides calories.
- Treatment of complications – Issues like infections, cysts, or diabetes may need targeted therapies.
- Surgery – Surgery may be required to remove gallstones or drain pseudocyst in severe cases.
Mild acute pancreatitis often resolves on its own within a week with proper treatment. More severe cases can involve a prolonged hospital stay.
With chronic pancreatitis, the goal is to manage symptoms long-term since there is no cure. This may involve taking pancreatic enzyme supplements, controlling blood sugar, and avoiding triggers like alcohol.
Prevention for Pancreatitis and Diabetes
Preventing pancreatitis and diabetes involves being proactive about your health. While you can’t control everything, there are some key steps you can take to reduce your risks
here are tips for preventing pancreatitis and diabetes in a simple table:
| Prevention Tips for Pancreatitis | Prevention Tips for Diabetes |
|---|---|
| Avoid heavy/binge drinking | Maintain healthy body weight |
| Limit alcohol to 1 drink/day women, 2/day men | Eat a balanced diet with whole foods |
| Use caution with medications that can harm pancreas | Limit sweets, refined carbs, sugary drinks |
| Get treatment promptly for gallstones or high triglycerides | Stay active with cardio and strength training |
| Get blood sugar tested if at risk | |
| Control prediabetes through lifestyle changes | |
| Take all prescribed diabetes medications | |
| Check blood sugar routinely | |
| Aim for optimal glucose levels | |
| Get regular medical care |
Conclusion: Take a Proactive Approach
As you can see, pancreatitis and diabetes have an interwoven relationship where each condition influences the other. Pancreatitis can damage insulin-secreting cells and make diabetes more likely to develop and harder to control. Meanwhile, diabetes predisposes people to inflammation of the pancreas.
If you have either condition, it’s important to be vigilant about early symptom recognition and proactive treatment. Work closely with your medical providers to control risk factors, monitor blood sugar routinely, avoid pancreatitis triggers like alcohol, and take all prescribed medications. Catching and managing problems early is key to preventing complications with your pancreas and diabetes.
Frequently Asked Questions
Is diabetes related to pancreatitis?
Yes, there is a relationship between diabetes and pancreatitis. Pancreatitis causes inflammation of the pancreas, which can damage insulin-producing cells. This makes it harder for the body to produce enough insulin to control blood sugar levels. As a result, pancreatitis increases the risk of developing diabetes. The opposite is also true – diabetes seems to raise the chances of getting pancreatitis since high blood sugar can damage the pancreas over time.
How do you treat diabetes secondary to pancreatitis?
The major goals are controlling blood sugar levels through medication, diet, and lifestyle changes. Insulin therapy or oral medications that increase insulin production or improve sensitivity may be prescribed. Eating smaller, frequent meals with nutrient-dense whole foods can help stabilize blood sugar. Getting pancreatitis under control through proper treatment is also key to improving the function of insulin-producing cells.
What is the relationship between the pancreas and diabetes?
The pancreas produces insulin, which is the hormone needed to regulate blood sugar. Diabetes results when the pancreas doesn’t produce enough insulin, or the body becomes resistant to insulin. Diseases like pancreatitis that damage the pancreas can impair insulin production and increase the risk of diabetes. Managing conditions that affect the pancreas is crucial for diabetes prevention and control.
Is chronic pancreatitis a risk factor for diabetes?
Yes, chronic pancreatitis definitely increases your risk of developing diabetes. The persistent inflammation damages insulin-secreting cells in the pancreas over time. One study found people with chronic pancreatitis were almost 4 times more likely to develop diabetes compared to the general population. Getting proper treatment and stopping pancreatitis progression is important to help reduce diabetes risk.