Pancreatitis Causes, Symptoms, and Treatment
The Ultimate Guide to Understanding Pancreatitis Causes, Symptoms, and Treatment
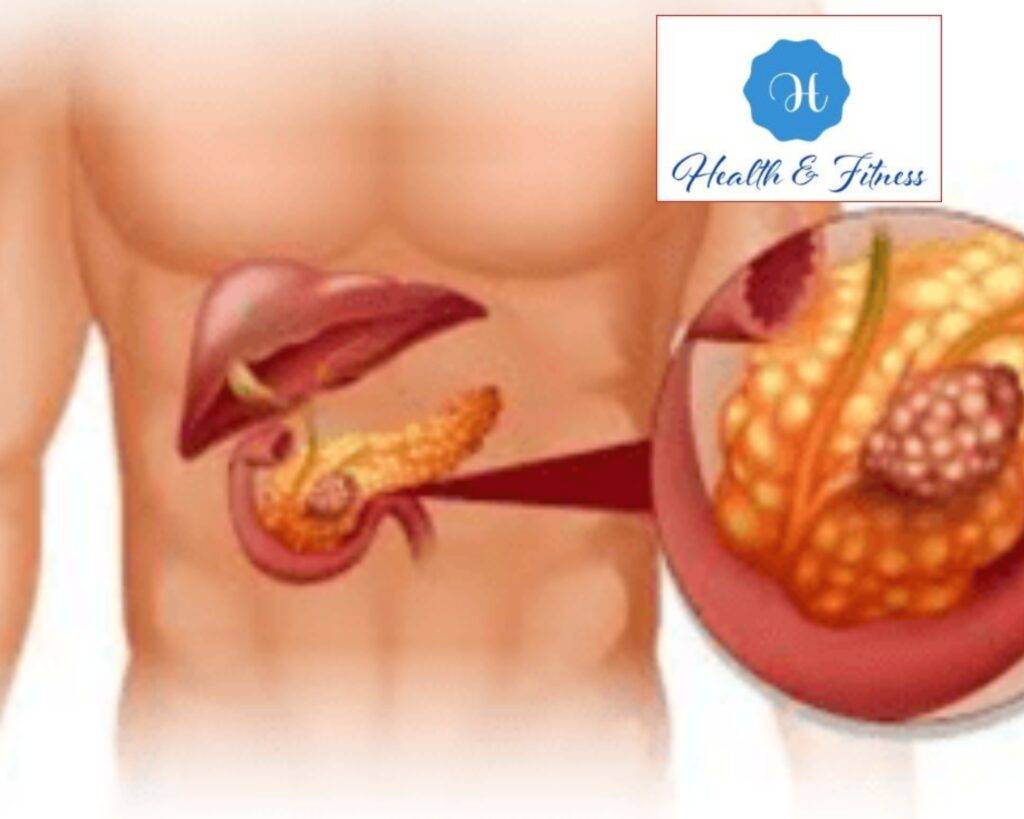
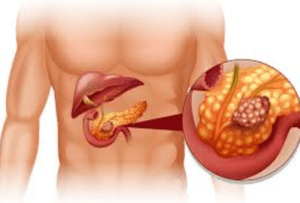
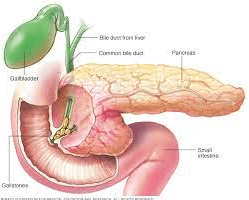
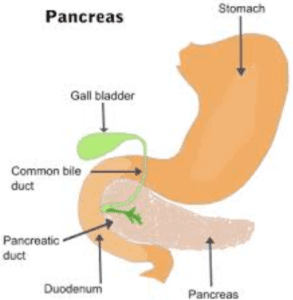
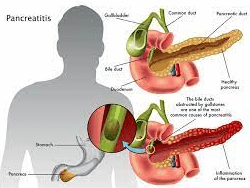
Explore Pancreatitis: Causes, Symptoms, and Treatment in our Comprehensive Guide. Learn About This Condition to Take Control of Your Health. Pancreatitis Causes, Symptoms, and Treatment – Pancreatitis refers to the inflammation of the pancreas when it becomes swollen and painful. The pancreas in the abdominal area produces enzymes and hormones that aid digestion and regulate blood glucose levels.
Inflammation of the pancreas can trigger pancreatitis, which may have varying degrees of severity, ranging from mild to life-threatening, and necessitates medical intervention. Understanding pancreatitis’s causes, symptoms, and treatment is essential to manage the condition effectively.
This guide aims to provide a comprehensive overview of pancreatitis. We will discuss the different types of pancreatitis, their causes, their symptoms, and how they are diagnosed. We will also cover treatment options and prevention strategies. Whether you are living with pancreatitis or seeking information to support a loved one, this guide will equip you with the knowledge you need to understand this condition.
Pancreatitis Causes –
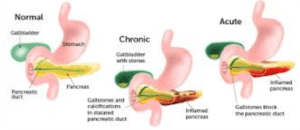
Additionally, Pancreatitis is caused by inflammation of the pancreas, which various factors can trigger. Pancreatitis is classified into two types: acute and chronic. Acute pancreatitis is a sudden pancreatic inflammation that resolves in a few days with proper treatment. Chronic pancreatitis is a long-term inflammation that can cause lasting harm and complications.
- Acute pancreatitis
- Gallstones
One of the most common causes of acute pancreatitis is gallstones. Gallstones are hard deposits in the gallbladder and can block the bile duct, leading to inflammation.
- Alcohol consumption
Heavy alcohol consumption is another common cause of acute pancreatitis. Alcohol irritates the pancreas and can cause inflammation.
- Trauma or injury to the pancreas
Trauma or injury to the pancreas, such as a car accident or a fall, can cause acute pancreatitis.
- Medications
Some drugs, including antibiotics, thiazide diuretics, and steroids, can make some individuals develop acute pancreatitis.
- High levels of triglycerides
High blood lipid levels can also cause acute pancreatitis.
Chronic pancreatitis
- Alcohol consumption
Heavy alcohol use over an extended period is the most typical cause of chronic pancreatitis.
Alcohol consumption can harm the pancreas over time and result in persistent inflammation.
- Genetics
Some genetic mutations can increase the risk of developing chronic pancreatitis. These mutations can affect the production and secretion of enzymes by the pancreas, leading to inflammation.
- Autoimmune disease
By causing pancreatic inflammation, autoimmune conditions, including lupus and rheumatoid arthritis, can lead to chronic pancreatitis.
- Cystic fibrosis
Cystic fibrosis is a genetic disorder that affects mucus production and can lead to chronic pancreatitis.
- High levels of calcium in the blood
Hypercalcemia, or elevated blood calcium levels, can cause calcium deposits in the pancreas, leading to chronic pancreatitis. Recognizing the root causes of pancreatitis is crucial for accurate diagnosis and treatment. If you suspect pancreatitis, seek medical attention right away. The following section will cover symptoms and diagnoses.
Symptoms of Pancreatitis: Causes
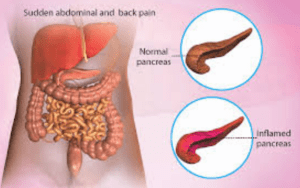
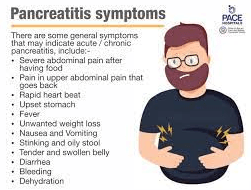
The symptoms of pancreatitis can vary depending on the severity and type of the condition. Acute pancreatitis may cause sudden and severe symptoms, while chronic pancreatitis may evolve. Here are the common symptoms of pancreatitis:
- Acute pancreatitis
- Upper abdominal pain
The most common symptom of acute pancreatitis is severe upper abdominal pain.
The pain may be sudden, intense, continuous, or intermittent, radiating to the back or chest.
- Nausea and vomiting
Acute pancreatitis can cause nausea, vomiting, and loss of appetite.
- Fever
Fever is another common symptom of acute pancreatitis. The fever may be low-grade or high, depending on the severity of the inflammation.
- Rapid pulse
Acute pancreatitis may cause an increase in heart rate or tachycardia.
- Swollen abdomen
In severe cases, acute pancreatitis can cause abdominal swelling and tenderness.
Chronic pancreatitis
- Upper abdominal pain
Like acute pancreatitis, chronic pancreatitis can also cause upper abdominal pain. However, the pain is usually less severe and may become constant over time.
- Weight loss
Chronic pancreatitis can cause weight loss because of a lack of appetite and difficulty digesting food.
- Nausea and vomiting
Nausea and vomiting may also occur in chronic pancreatitis.
- Steatorrhea
Steatorrhea is a condition in which the body cannot digest and absorb fats properly, resulting in loose, oily, and foul-smelling stools.
- Jaundice
Rarely, an obstruction in the bile duct caused by chronic pancreatitis can result in jaundice and yellowing of the skin and eyes.
It is critical to get medical help immediately if you encounter any pancreatitis symptoms.
The following section will discuss how pancreatitis is diagnosed and what tests may be performed.
Diagnosis of Pancreatitis
Pancreatitis can be diagnosed through physical exams, medical history, and laboratory tests.
Your doctor may also perform imaging tests to examine the pancreas and surrounding organs. Here are some standard diagnostic tests for pancreatitis:
- Medical history and physical exam
Your doctor will conduct a physical examination and ask questions about your medical history to look for symptoms of pancreatitis, such as abdominal discomfort and pain.
- Blood tests
Blood tests can help diagnose pancreatitis by measuring levels of enzymes produced by the pancreas.
High levels of these enzymes, such as amylase and lipase, can indicate pancreas inflammation.
- Imaging tests
- Ultrasound
An ultrasound is a non-invasive imaging test that uses sound waves to produce images of the pancreas and surrounding organs.
- CT scan
An imaging examination called a computed tomography (CT) scan creates fine-grained images of the pancreas and other organs using X-rays and computer technologies.
- Magnetic resonance imaging (MRI)
MRI is another imaging test that uses a magnetic field and radio waves to produce detailed images of the pancreas and surrounding organs.
- Endoscopic retrograde cholangiopancreatography (ERCP)
ERCP is an invasive test that combines endoscopy and X-rays to examine the pancreas and bile ducts. This test is typically reserved for cases where other tests have not provided a precise diagnosis.
- Biopsy
In rare cases, a biopsy may be performed to examine the pancreatic tissue for signs of inflammation or cancer.
It is essential to diagnose pancreatitis early to prevent complications and improve treatment outcomes.
If you experience any symptoms of pancreatitis, consult your doctor immediately.
In the next section, we will discuss the treatment options for pancreatitis.
Treatment of Pancreatitis:
The treatment of pancreatitis depends on the severity and type of the condition.
Mild cases of acute pancreatitis can usually be treated with rest, pain relief, and fluids, while severe cases may require hospitalization and surgery.
Chronic pancreatitis is typically managed with long-term medical care to relieve symptoms and prevent complications. Here are some standard treatment options for pancreatitis:
-
Acute pancreatitis
- Hospitalization
Severe cases of acute pancreatitis may require hospitalization to manage pain, provide intravenous fluids, and monitor for complications.
- Pain relief
Pain relief is a critical component of treating pancreatitis.
Your doctor may prescribe pain medications like acetaminophen, ibuprofen, or opioids.
- NPO (Nothing by Mouth)
In severe cases, your doctor may recommend NPO, or nothing by mouth, to rest the pancreas and prevent further inflammation.
- Intravenous fluids
Intravenous fluids may be used to replace fluids lost because of vomiting or to prevent dehydration.
- Nutritional support
Once symptoms have improved, your doctor may recommend a gradual return to a regular or special diet high in protein and low in fat.
-
Chronic pancreatitis
- Pain management
Chronic pancreatitis can cause long-term pain that may require pain management with medications.
- Nutritional support
A low-fat, high-protein diet may help reduce symptoms of chronic pancreatitis.
- Enzyme supplements
Enzyme supplements can help the body digest food properly and reduce symptoms of malabsorption.
- Insulin therapy
If chronic pancreatitis has caused damage to the cells that produce insulin, insulin therapy may be needed to control blood sugar levels.
- Surgery
In severe cases of pancreatitis, surgery may be necessary to remove damaged tissue or drain fluid or pus from the pancreas or surrounding areas. However, working closely with your doctor to develop a treatment plan that works best for you is essential. Most people with pancreatitis can manage their symptoms and prevent complications with proper treatment. The following section will discuss some lifestyle changes that may help prevent pancreatitis.
Prevention of Pancreatitis Causes
While not all cases of pancreatitis can be prevented, you can make some lifestyle changes to reduce your risk of developing the condition.
Here are some tips for preventing pancreatitis:
- Limit alcohol consumption
Alcohol is a common cause of pancreatitis, particularly chronic pancreatitis.
Limiting alcohol consumption or avoiding it altogether can reduce your risk of developing pancreatitis.
- Maintain a healthy weight.
Being overweight can increase your risk of developing pancreatitis.
Maintaining a healthy weight through regular exercise and a balanced diet can reduce your risk.
- Quit smoking
Smoking increases your chances of acquiring pancreatitis and other major health problems.
Smoking cessation can lower your risk and enhance your overall health.
- Manage underlying health conditions.
Certain health conditions, such as high triglyceride levels or gallstones, can increase your risk of developing pancreatitis.
Managing these conditions with medication and lifestyle changes can reduce your risk.
- Avoid certain medications
Some medications, such as corticosteroids and certain antibiotics, can increase your risk of developing pancreatitis.
Avoiding these medications when possible can reduce your risk.
- Follow a healthy diet.
Eating a healthy diet low in fat and high in protein can reduce your risk of developing pancreatitis.
Avoiding high-fat foods and processed foods can help prevent inflammation of the pancreas.
By making these lifestyle changes, you can reduce your risk of developing pancreatitis and improve your overall health. If you have questions or concerns about pancreatitis, consult your doctor.

Conclusion
Most people with pancreatitis can manage their symptoms and prevent complications with proper diagnosis and treatment.
To prevent pancreatitis, make healthy lifestyle choices like limiting alcohol, maintaining a healthy weight, quitting smoking, managing underlying health conditions, avoiding certain medications, and following a healthy diet.
If you experience symptoms, seek medical attention right away.
Boost Your Vitamin D Levels with These Top 15 Foods: A Comprehensive Guide

Adel Galal is a health and wellness writer with over 30 years of experience studying and writing about health, fitness, nutrition, and healthy living. He is the founder of NextFitLife.com, where he shares practical, evidence-based guidance to support long-term health at any age. Adel’s mission is simple:
to help people make smarter health choices that fit real life, at any age.