Weight Loss Surgery on the NHS: Everything You Need to Know to Make an Informed Decision
Considering Weight Loss Surgery NHS? Get Informed! Everything You Need to Know for a Confident Decision. Explore Now
Introduction to Weight Loss Surgery NHS
Weight loss surgery NHS, or bariatric surgery, is a surgical procedure designed to help people who are severely overweight lose weight and improve their overall health. It is not a fast cure, but it may help you lose weight and improve your health. If you’re contemplating weight reduction surgery, you should know your choices, risks, and advantages. This blog article covers NHS weight loss surgery eligibility, kinds of surgery, risks, and benefits, and long-term lifestyle modifications to sustain weight reduction. This article will help you comprehend weight loss surgery and decide whether it’s right for you.
Understanding Weight Loss Surgery NHS and How it Works

Weight loss surgery alters digestion to limit food intake and nutrient absorption. There are two types: restrictive (e.g., LAGB, sleeve gastrectomy) and malabsorptive (e.g., RYGB, BPD-DS). Under general anesthesia, these hospital-based procedures depend on health, BMI, and pre-op exams. While not a quick fix, they aid weight loss and health improvement, requiring post-op lifestyle changes and medical follow-up. Next, we explore NHS eligibility for weight reduction surgery.
Eligibility Criteria for Weight Loss Surgery NHS

NHS weight reduction surgery requires specific qualifying conditions. These requirements vary for each procedure but usually include the following:
- A body mass index (BMI) of 40 or more or a BMI of 35 or more with one or more fat-related health problems, such as type 2 diabetes or high blood pressure.
- A history of attempted weight loss through non-surgical means, such as diet and exercise, for at least 12-24 months before surgery.
- A commitment to making long-term lifestyle changes, including a healthy diet and regular exercise, to maintain weight loss after surgery.
- No significant psychological or medical conditions that would make surgery unsafe or increase the risk of complications.
- A willingness to undergo a thorough pre-operative evaluation may include psychological and nutritional assessments and medical testing to ensure that the patient is healthy enough for surgery.
Meeting qualifying requirements does not ensure NHS weight reduction surgery approval. A multidisciplinary team of healthcare specialists evaluates the patient’s health and the procedure’s risks and advantages before approving or denying surgery.
What Kinds of Weight Loss Surgery NHS Offer?
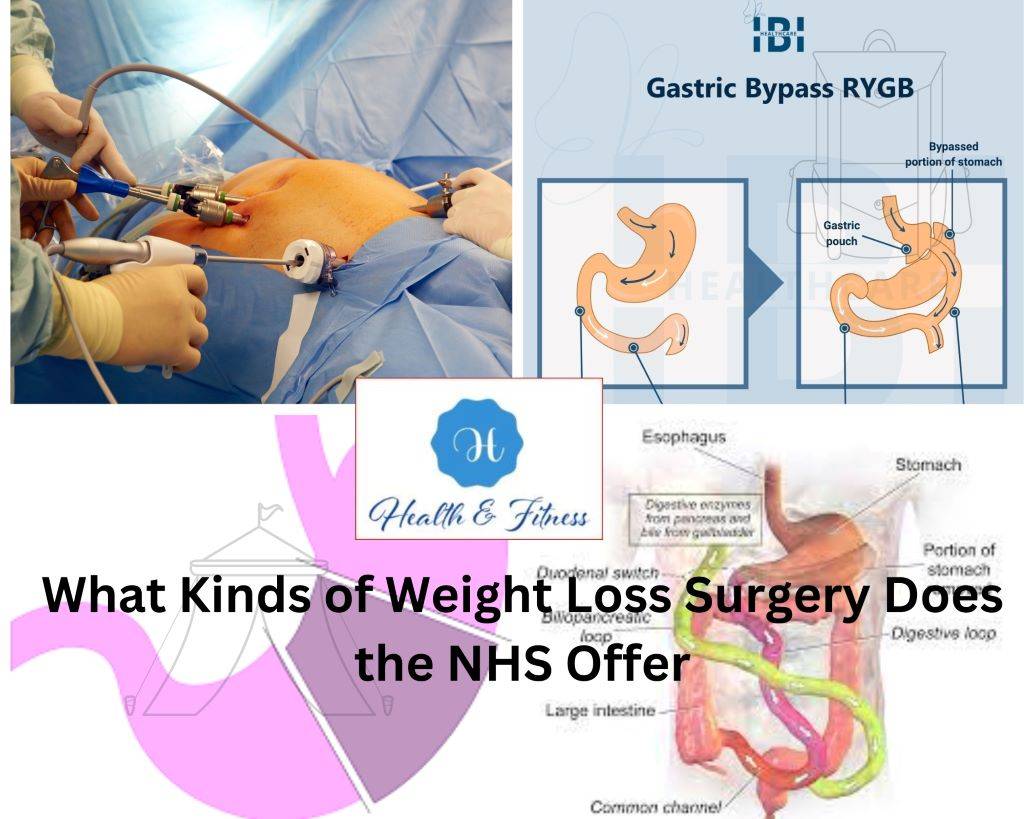
The NHS offers a variety of weight loss surgeries, each with its advantages and disadvantages. On the NHS, the most frequent procedures for weight loss are:
- Adjustable gastric bands placed laparoscopically
This surgery wrapped a plastic band around the top of the stomach. This makes a small pouch that can only hold a handful of food. The band can be changed so that you can control how quickly food moves through your stomach. This can help you lose weight.
- RYGB stands for Roux-en-Y gastric bypass.
This surgery involves dividing the stomach into a small upper pouch and a larger lower pouch and then connecting the upper pouch directly to the small intestine. This bypasses part of the stomach and small intestine, reducing the amount of calories and nutrients absorbed by the body.
- Sleeve gastrectomy
This surgery removes a large portion of the stomach, leaving a small sleeve-shaped section that can hold only a tiny amount of food. This reduces the amount of food consumed at anyone time and promotes weight loss.
- Duodenal switch after biliopancreatic rerouting (BPD-DS)
In this procedure, we redirect the small intestine to avoid the stomach, removing a significant section of the intestine. This reduces the amount of calories and nutrients that are absorbed by the body. Each weight reduction surgery has risks and advantages; the patient’s circumstances and objectives will determine their chosen operation. Choosing the correct procedure requires a comprehensive consultation with a healthcare specialist.
Risks and Benefits of Weight Loss Surgery NHS
NHS weight loss surgery can reduce obesity but has risks and problems.
Advantages and risks:
Benefits:
- Rapid and long-term weight loss
Patients with Metabolic surgery may shed a large amount of weight and keep it off over the long term with the help of the procedure.
- Improved obesity-related health conditions
Weight loss surgery has been shown to treat or even cure several obesity-related health conditions, such as type 2 diabetes, high blood pressure, and sleep apnea.
- Improved quality of life
After weight loss surgery, many people find that they can move around, have more self-confidence, and feel healthier.
Risks and potential complications:
- Infection: All surgery carries a risk of infection, which can be a severe and life-threatening complication.
- Bleeding: Weight loss surgery can cause bleeding during and after the procedure, which may require further medical intervention.
- Blood clots: Weight loss surgery increases the risk of blood clots forming in the legs or lungs, which can be a severe and life-threatening complication.
- Nutritional deficiencies: Weight loss surgery can interfere with the body’s ability to absorb nutrients, leading to deficiencies in essential vitamins and minerals.
- Need for further surgery: Some patients may require additional surgeries to correct complications or adjust the initial surgery.
- Psychological effects: Weight loss surgery can have psychological effects, such as depression or anxiety, which may require additional treatment or support.
Before choosing NHS weight reduction surgery, individuals should carefully examine the risks and benefits and talk with a healthcare practitioner to be sure the operation is correct.
Preparing for Weight Loss Surgery NHS: What to Expect
Patients should know that NHS weight reduction surgery preparation might take a long time. NHS weight reduction surgery preparation includes:
- Initial consultation
The first step is typically with a healthcare professional, who will review the patient’s medical records to see if they qualify for NHS weight loss surgery.
- Referral to a specialized medical facility
If the patient qualifies for weight loss surgery, they will be referred to a specialized facility for evaluation and treatment.
- Pre-operative assessment
Patients will receive blood, imaging, and other diagnostic testing before surgery to guarantee their health.
- Diet and exercise before surgery
Patients are often instructed to stay true to a specified diet and exercise plan in the days and weeks before surgery to facilitate a quick recovery.
4. Hospital admission
Patients will be admitted and undergo the procedure under general anesthesia on the day of the surgery.
5. Post-operative care
After the surgery, patients must follow a strict post-operative care plan, including pain management, wound care, and a specific diet and exercise regimen.
6. Follow-up care
Regular follow-up care with healthcare professionals is essential to monitor progress, address complications, or concerns, and ensure long-term success. With the correct help and counselling, people may prepare for NHS weight reduction surgery. To get the most outstanding results, communicate openly with healthcare experts.
The Weight Loss Surgery NHS Procedure: Step-by-Step
The NHS weight reduction surgery technique varies by kind. However, there are certain common elements.
As follows :
- Anesthesia: The patient will be given general anesthesia, which will put them to sleep for the duration of the procedure.
- Incision: The surgeon will make one or more small incisions in the abdomen to access the stomach.
- Laparoscopic instruments: The surgeon will use laparoscopic instruments, which are small, specialized tools that allow for precise movements within the abdomen.
- Surgery: Depending on the type of surgery being performed, the surgeon will then either remove a portion of the stomach, create a small pouch at the top of the stomach, or reroute the small intestine.
- Closing incisions: The surgeon will close the surgery with sutures or staples once the surgery is complete.
- Recovery room: The patient will be taken to a recovery room and monitored closely as they wake up from the anesthesia.
- Hospital stay: Depending on the type of surgery and the patient’s circumstances, they may need to stay there several days after the procedure.
- Post-operative care: After leaving the hospital, the patient must follow a strict post-operative care plan, including pain management, wound care, and diet and exercise regimen.
- Follow-up care: Regular follow-up care with healthcare professionals is essential to monitor progress, address complications or concerns, and ensure long-term success.
NHS weight loss surgery is a severe treatment with risks and repercussions. Before choosing surgery, patients should weigh the pros and drawbacks and check with a doctor to be sure it’s right for them.
Recovery After Weight Loss Surgery NHS: Tips and Advice
NHS weight loss surgery recovery is hard. Follow your doctor’s post-op care regimen to recover correctly and lose weight. Here are some NHS weight reduction surgery recovery tips:
- Follow dietary guidelines
After weight loss surgery on the NHS, patients must follow a strict diet plan to promote healing and weight loss. For the first few days, the diet will consist of clear liquids, then solid foods over several weeks. Patients should follow their doctor’s diet and avoid meals and drinks that cause discomfort or slow healing.
- Stay active
After NHS weight reduction surgery, individuals must remain active. Walking helps circulation, prevents blood clots, and speeds recovery. Healthcare providers should advise patients on safe physical activity resumption.
- Manage pain
NHS weight loss surgery causes pain.
Talk to your doctor or nurse about pain treatment, including over-the-counter and prescription medicines.
If the discomfort persists, patients should contact their doctor.
- Attend follow-up appointments
NHS weight reduction surgery requires regular medical follow-ups. These checkups let doctors check progress, resolve issues, and alter post-op treatment.
- Seek emotional support
NHS weight reduction surgery may induce anxiety, depression, and other emotional illnesses. Family, friends, support groups, and mental health professionals should help patients emotionally. NHS weight loss surgery recovery is lengthy and arduous, but with help, individuals may lose weight and improve their health.
Long-term Lifestyle Changes After Weight Loss Surgery NHS
NHS weight reduction surgery may change your life, but it’s not a miracle. Weight reduction and health improvement need long-term lifestyle adjustments. Post-NHS weight reduction surgery lifestyle modifications include:
- Follow a healthy diet: After Obesity surgery, patients must follow a healthy diet plan to maintain weight loss and promote overall health. Patients should consume foods high in protein, fiber, and nutrients and limit processed foods, sugary drinks, and high-fat foods. Patients should also avoid snacking between meals and consuming large portions.
- Stay active: Physical activity is essential for maintaining weight loss and promoting overall health. Patients should aim to engage in regular physical activity, such as walking, swimming, or cycling. As healthcare professionals recommend, patients should aim for at least 150 minutes of moderate physical activity per week.
- Attend support groups: Support groups can be an excellent resource for patients after weight loss surgery on the NHS. Support groups provide a safe and supportive environment where patients can share their experiences, ask questions, and receive advice and encouragement from other patients who have undergone weight loss surgery.
- Practice self-care: After weight loss surgery on the NHS, patients must prioritize self-care to maintain physical and emotional health. Patients with anxiety, depression, or other emotional difficulties should practice yoga or meditation and seek expert counselling.
- Attend follow-up appointments: Regular follow-up appointments with healthcare professionals are essential after weight loss surgery on the NHS. These appointments allow healthcare professionals to monitor progress, address complications, or concerns, and adjust the post-operative care plan.
With determination and assistance, people may lose weight and improve their health following NHS weight reduction surgery.
Frequently Asked Questions About Weight Loss Surgery NHS
- Who is eligible for weight loss Gastric surgery?
NHS weight reduction surgery is available to anyone with a BMI of 40 or higher or 35 or higher with at least one weight-related health issue, such as diabetes or high blood pressure.
- What types of weight loss surgery are available on the NHS?
Gastric band, bypass, and sleeve gastrectomy surgeries are available on the NHS.
- What risks are associated with weight loss surgery on the NHS?
NHS weight loss surgery risks bleeding, infection, and blood clots. Dietary and digestive problems are long-term concerns.
- What are the benefits of weight loss Gastric surgery?
Gastric surgery improves the quality of life, weight loss, and weight-related health issues like diabetes and high blood pressure.
- How long does it take to recover from weight loss for Obesity surgery?
Gastric surgery recovery depends on health. Most individuals may return to work two to four weeks after surgery, but complete recovery may take months.
- Will I need to make lifestyle changes after weight loss surgery on the NHS?
Yes, NHS weight loss surgery helps people lose weight. Maintaining weight reduction and health requires lifelong adjustments, like regular exercise and a healthy diet.
Conclusion
Obese patients can change their lives with NHS weight loss surgery. It can help you lose weight and improve your health, but it requires major lifestyle changes. Before pursuing this option, eligibility criteria, risks, and benefits, and long-term lifestyle changes should be weighed. Speak with your GP or healthcare provider to discuss whether weight loss surgery on the NHS is right for you.
References:
- National Health Service (NHS). (2021). Weight loss (bariatric) surgery. Retrieved from https://www.nhs.uk/conditions/weight-loss-surgery/
- American Society for Metabolic and Bariatric Surgery. (n.d.). Benefits of weight loss surgery. Retrieved from https://asmbs.org/patients/benefits-of-weight-loss-surgery
- National Institute for Health and Care Excellence (NICE). (2014). Obesity: identification, assessment, and management. Retrieved from https://www.nice.org.uk/guidance/cg189