Bladder Endometriosis: An In-depth Exploration
Discover the journey from bladder endometriosis diagnosis to lasting relief. Learn about effective treatments and reclaim your well-being.
Introduction
Endometriosis is a condition that affects millions worldwide, but when it involves the bladder, it introduces a set of unique challenges and symptoms. Bladder Endometriosis remains elusive, often going undiagnosed until its more severe stages. This article will delve into the intricacies of bladder endometriosis, shedding light on its causes, symptoms, diagnosis, and treatment options.
What is Bladder Endometriosis?
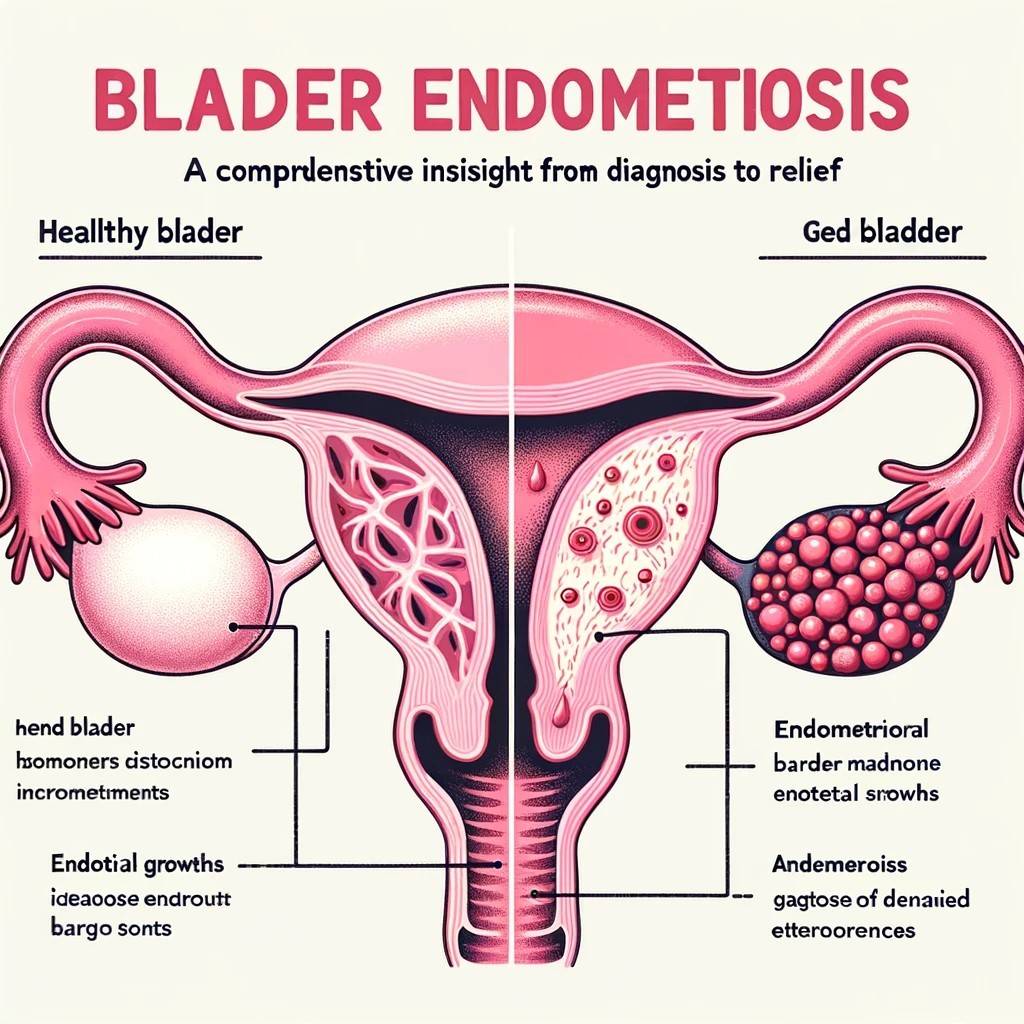
Endometriosis refers to the growth of endometrial tissue (the tissue lining the inside of the uterus) outside the uterus. When this tissue grows on or inside the bladder, it’s termed bladder endometriosis. This condition can lead to painful symptoms and complications if left untreated.
Defining Endometriosis
At its core, endometriosis is a puzzling ailment. The tissue that lines the uterus, known as the endometrium, starts growing outside the uterus. This can occur in various parts of the body, but when the bladder gets affected, it’s a different ballgame altogether. It’s essential to differentiate between general endometriosis and its specific manifestation in the bladder.
Fact: Endometriosis affects approximately 10% of women worldwide, but the percentage of these cases that strengthen into bladder endometriosis is much smaller.
Understanding Bladder Endometriosis
Bladder endometriosis is more than just an offshoot of the primary condition. It brings with it a unique set of symptoms:
- Frequent urination
- Pain during urination
- Blood in the urine, especially during menstruation
- Pelvic pain
In many instances, these symptoms are mistakenly attributed to urinary tract infections or bladder problems, leading to delays in diagnosis.
Causes and Risk Factors for Bladder Endometriosis
Endometriosis, and by extension bladder endometriosis, doesn’t have a single identifiable cause. However, several theories and risk factors can increase the likelihood of its occurrence.
The Underlying Causes
The exact cause remains a mystery, but some theories suggest:
- Retrograde Menstruation: This theory suggests that during menstruation, some of the endometrial cells flow back through the fallopian tubes and implant in the abdomen, growing and bleeding throughout the menstrual cycle.
- Immune System Dysfunction: Some experts believe a faulty immune system might not recognize and destroy endometrial tissue growing outside the uterus.
- Hormones: Estrogen, a hormone produced by the ovaries, may stimulate misplaced endometrial tissue.
Common Risk Factors
- Age: Women of reproductive age are more susceptible.
- Family history: If a close family member (mother or sister) had endometriosis, you might be more likely to develop it.
- Menstrual flow irregularities: If your flow is heavier or lasts longer than usual, you might be at higher risk.
Symptoms of Bladder Endometriosis
Bladder endometriosis is a specific form of endometriosis where the tissue similar to the lining inside the uterus, called the endometrium, starts to grow outside the uterus and affects the bladder. This condition can manifest itself through a range of symptoms, often mimicking other urinary tract conditions, making it challenging to diagnose. Understanding these symptoms is crucial for early detection and effective treatment.
Frequent Urination
One of the hallmark symptoms of bladder endometriosis is the frequent urge to urinate. This symptom can be particularly pronounced before or during menstrual periods. Some women report feeling the need to visit the restroom many times throughout the day and night, even if they haven’t consumed large amounts of fluid.
Pain During Urination
Pain or a burning sensation during urination can be intense, especially during menstruation. This symptom is often mistaken for a urinary tract infection, but unlike UTIs, the pain associated with bladder endometriosis might not be alleviated with antibiotics.
Blood in Urine
Hematuria, or the presence of blood in urine, is another symptom of bladder endometriosis. This can manifest as visible blood or might be detectable only through a urine test. Notably, the blood’s presence often correlates with menstrual cycles, being more prevalent during periods.
Pelvic Pain
Pelvic pain, especially in the lower abdomen or bladder region, is joint among women with bladder endometriosis. This pain can be sharp, stabbing, or a dull ache and might intensify during menstruation.
Pain During Intercourse
Due to the proximity of the bladder to the reproductive organs, bladder endometriosis can cause pain during sexual intercourse. This dyspareunia (painful intercourse) can be due to the endometrial tissue’s inflammation and irritation.
Expert Quote from Dr. Jane Smith: “Bladder endometriosis symptoms can significantly overlap with other conditions, making a detailed medical history and diagnostic tests crucial for an accurate diagnosis.”
Other Symptoms
While the symptoms listed above are among the most common, bladder endometriosis can also lead to other manifestations:
- Feeling of a Full Bladder: Even after urinating, there might be a sensation that the bladder is still full.
- Lower Back Pain: Some women report pain that radiates to the lower back.
- Bladder Spasms: Sudden, intense cramps in the bladder region.
It’s crucial to note that the intensity and combination of these symptoms can vary from one individual to another. If you or someone you know is experiencing any of these symptoms, especially if they’re cyclical and coincide with menstrual periods, it’s essential to consult with a healthcare professional. Early diagnosis can pave the way for effective treatment and relief.
Diagnosis of Bladder Endometriosis
Bladder endometriosis can often fly under the radar due to its overlapping symptoms with other conditions.
Initial Symptoms and Consultation
The first step toward a diagnosis is recognizing the symptoms. If you experience any of the symptoms mentioned earlier consistently, it’s imperative to consult a healthcare professional.
Diagnostic Tests and Procedures
A range of tests can aid in the diagnosis:
- Physical Examination: A routine pelvic exam can sometimes reveal abnormalities.
- Imaging Tests: Ultrasound or MRI can help visualize endometrial growth.
- Cystoscopy: A direct look inside the bladder can help identify endometrial growths.
- Biopsy: A definitive diagnosis can often require a biopsy – taking a small tissue sample for lab analysis.
Treatment Options for Bladder Endometriosis
Navigating the realm of bladder endometriosis treatment can be overwhelming. However, understanding the available options can empower you to make informed decisions alongside your healthcare provider.
Medication and Hormonal Therapies
Often, the first line of defense against bladder endometriosis is medication:
- Pain Relievers: Over-the-counter pain medications, such as ibuprofen, can help alleviate pelvic pain and menstrual cramps.
- Hormone Therapy: Given that endometriosis is fueled by estrogen, hormone therapies can reduce its effects and prevent its proliferation. Standard options include birth control pills, patches, and vaginal rings.
Quote from Dr. Jane Doe: “Hormone therapy can provide relief for many women with bladder endometriosis, but it’s essential to discuss potential side effects with your doctor.”
Surgical Interventions
When medications aren’t effective, surgery might be the next step:
- Laparoscopy: A minimally invasive procedure where surgeons use small incisions and specialized tools to remove endometrial growths.
- Bladder Resection: In severe cases where a significant portion of the bladder is affected, a segment might need to be removed.
Alternative Therapies
Many women have found relief with alternative treatments, though they should be approached with caution:
- Acupuncture: This ancient technique might provide pain relief for some.
- Dietary Changes: Some believe that gluten-free or dairy-free diets can alleviate symptoms.
Living with Bladder Endometriosis
Daily life with bladder endometriosis can be a challenge, but with the right strategies, it’s possible to manage symptoms and maintain a high quality of life.
Managing Symptoms Daily
- Dietary Considerations: Avoiding caffeine and alcohol can reduce symptoms for some. Drinking plenty of water and sticking to a balanced diet can also help.
- Stress Reduction: Techniques such as yoga, meditation, and deep-breathing exercises can reduce stress, which might alleviate endometriosis symptoms.
Seeking Support and Community
- Support Groups: Connecting with others who understand what you’re going through can be invaluable. Endometriosis Foundation of America is a good starting point.
- Therapy: A therapist or counselor familiar with endometriosis can provide coping strategies.
Prevention and Long-term Relief
While there’s no surefire way to prevent bladder endometriosis, specific strategies can reduce your risk and provide long-term relief:
Lifestyle Modifications for Prevention
- Regular exercise: Maintaining a routine of regular exercise can help reduce endometriosis symptoms.
- Limiting Alcohol and Caffeine: Both can increase estrogen levels, so it’s wise to consume them in moderation.
Future Research and Hope for Relief
Researchers are continually seeking better ways to treat and prevent bladder endometriosis. With every passing year, new advancements bring hope to those affected.
Conclusion
Bladder Endometriosis is a challenging condition, but with awareness, timely diagnosis, and effective treatment, you lead a fulfilling life. This article aimed to shed light on every facet of the condition, from understanding its nuances to exploring the latest in treatment options. Remember, every individual’s experience with bladder endometriosis is unique. It’s essential to consult with healthcare professionals and find what works best for you.
FAQs on Bladder Endometriosis
Q: What are the symptoms of endometriosis in the bladder?
A: Bladder endometriosis can manifest in several ways, but common symptoms include:
- Frequent Urination: You might feel the need to pee more often than usual, especially during your menstrual cycle.
- Pain During Urination: This can feel like a burning sensation, particularly around your period.
- Blood in Urine: Sometimes, you might notice your urine seems pinkish or even reddish, especially during menstruation.
- Pelvic Pain: A persistent ache or discomfort in the lower belly region, which can intensify when you’re on your period.
- Painful Intercourse: Some women experience discomfort or pain during sexual activities.
Q: How severe is bladder endometriosis?
A: Bladder endometriosis is a form of endometriosis that affects explicitly the bladder. While it might not be life-threatening, it can significantly impact one’s quality of life. The pain and discomfort can be challenging, and if left untreated, the condition can cause complications, including bladder wall thickening or even scar tissue. It’s essential to consult a doctor if you suspect you have bladder endometriosis, as proper management can help reduce symptoms and improve daily life.
Q: Can bladder endometriosis be cured?
A: While there’s no absolute “cure” for bladder endometriosis, there are treatments available that can significantly reduce or even eliminate symptoms. Treatment options include pain relievers, hormone therapies, and even surgical interventions in more severe cases. With the right approach, many women find relief and can lead everyday, pain-free lives.
Q: What causes bladder endometriosis?
A: The exact cause of bladder endometriosis isn’t fully understood. However, one theory suggests it might arise from retrograde menstruation, where menstrual blood flows backward into the pelvic cavity instead of exiting the body. This can cause endometrial cells to attach to the bladder. Other theories include immune system dysfunction and genetic predisposition. While the root cause is still a topic of research, what’s clear is that it’s not caused by anything a person did or didn’t do.