
Stomach gurgling and gas for a week: Causes and Solutions Unveiled!
Stomach gurgling and gas for a week: Causes and Solutions

12 Best food for kids growth: Boost Height, Strength, and Brainpower Naturally
12 Best food for kids growth: Boost Height, Strength, and
Ab workouts for men: 15 Exercises to Sculpt a Shredded Core
Ab workouts for men: 15 Exercises to Sculpt a Shredded
Beauty

Best Acne Treatment for Teens: Teen-Friendly Solutions Unveiled
Best Acne Treatment for Teens: Teen-Friendly Solutions Unveiled Reveal Radiant
Aging Neck Solutions: 10 Habits to Maintain a Graceful Profile Forever!
Aging Neck Solutions: 10 Habits to Maintain a Graceful Profile

Lazy Eye Exercises Unveiled: Your Path to Clear Vision!
Lazy Eye Exercises Unveiled: Your Path to Clear Vision! Lazy

Vitamins for Skin and Hair: Transformative Beauty Secrets
Unlock Radiant Beauty: Explore the Transformative Secrets of Vitamins for

Rosemary Oil for Hair Growth Before and After: A Detailed Exploration
Rosemary Oil for Hair Growth Before and After: A Detailed

Best Skin Care for Men: Unleash Your Handsome Glow!
Best Skin Care for Men: Unleash Your Handsome Glow! Unleash

Diet for Glowing Skin in 3 Days: Your 72-Hour Glow-Up
Diet for Glowing Skin in 3 Days: Your 72-Hour Glow-Up

Rosemary Oil for Hair: 14 Surprising Benefits for Hair Growth
Rosemary Oil for Hair: 14 Surprising Benefits for Hair Growth
Foods

12 Best food for kids growth: Boost Height, Strength, and Brainpower Naturally
12 Best food for kids growth: Boost Height, Strength, and Brainpower Naturally Fuel your child’s growth with these 12 nutrient-packed
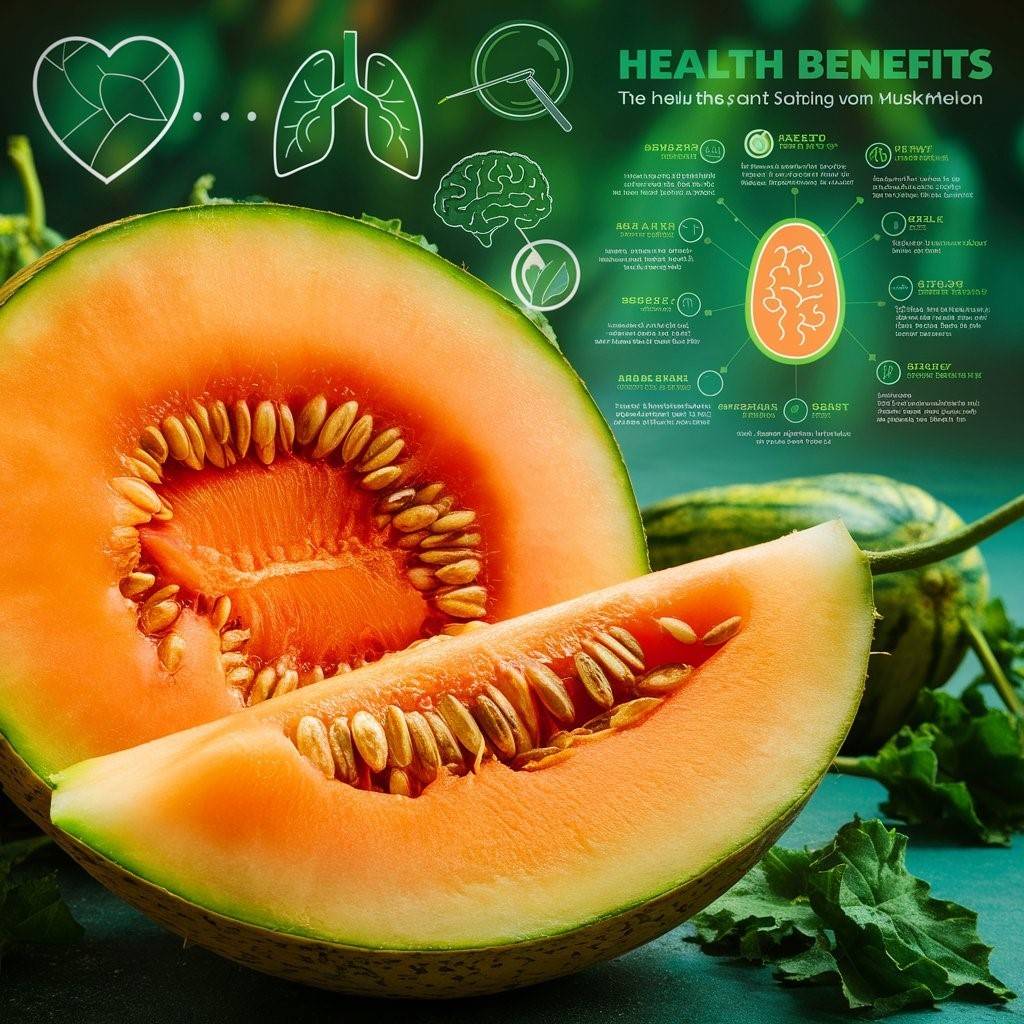
14 Muskmelon Benefits: The Sweet Superfood for Glowing Skin and Health
14 Muskmelon Benefits: The Sweet Superfood for Glowing Skin and Health Discover the amazing Muskmelon Benefits for glowing skin, better

Best food for kids constipation: Easy fixes for digestive woes
Best food for kids constipation: Easy fixes for digestive woes Discover the best food for kids constipation relief, including fiber-rich

15 Best Food for Kids: Smart Choices for Healthy, Happy Children!
15 Best Food for Kids: Smart Choices for Healthy, Happy Children! As parents, making sure our kids eat right is

How is Watermelon Good for You? Unveiling 10 Unexpected Advantages!
How is Watermelon Good for You? Unveiling 10 Unexpected Advantages! How is Watermelon Good for You? Discover the wonderful health

Dash Diet: Unlock the Secret to Lower Blood Pressure Today!
Dive into the Dash Diet: Your Key to Lowering Blood Pressure Today! Discover the power of the Dash Diet to

16 Foods to cut out for weight loss: The hidden calorie bombs
16 Foods to cut out for weight loss: The hidden calorie bombs. Discover 16 foods to cut out for
Explore health


Can Constipation Cause Nausea: Finding Relief and Answers

Bloating Gurgling Stomach: Causes, Symptoms, and Solutions


Fitness Tips

Top Exercises for Belly Fat: The Ultimate Fat-Burning Routine
Top Exercises for Belly Fat: The Ultimate Fat-Burning Routine Blast stubborn belly fat with the top exercises for belly fat.

Fitness Journey: Your Roadmap to Health, Happiness, and Strength
Fitness Journey: Your Roadmap to Health, Happiness, and Strength Beginning a “fitness journey” is an exciting adventure that can change

Best Weight Loss Options for Young Women: Empowering Your Journey to Wellness
Best Weight Loss Options for Young Women: Empowering Your Journey to Wellness Discover the best weight loss options for young

Getting Fit at 60: Creating a Safe and Effective Fitness Routine
Getting Fit at 60: Creating a Safe and Effective Fitness Routine Learn how to start Getting Fit at 60 with
Animals Health

How to Clean Dogs Ears: Unleash the Secrets to Happy Ears
How to Clean Dogs Ears: Unleash the Secrets to Happy

Dog Dementia Detectives: Solving the Mystery of Canine Memory Loss
Dog Dementia Detectives: Solving the Mystery of Canine Memory Loss

Dog Vomiting and Diarrhea: A Quick Owner’s Guide
Dog Vomiting and Diarrhea: A Quick Owner’s Guide Dealing


